Hypertension and chest pain and opiates and blood pressure
In the vast and complex landscape of public health, a nagging issue persists: the opiate crisis and its intertwined relationship with blood pressure regulation. As the epidemic continues to devastate communities nationwide, new research sheds light on the intricate links between these two critical health indicators.
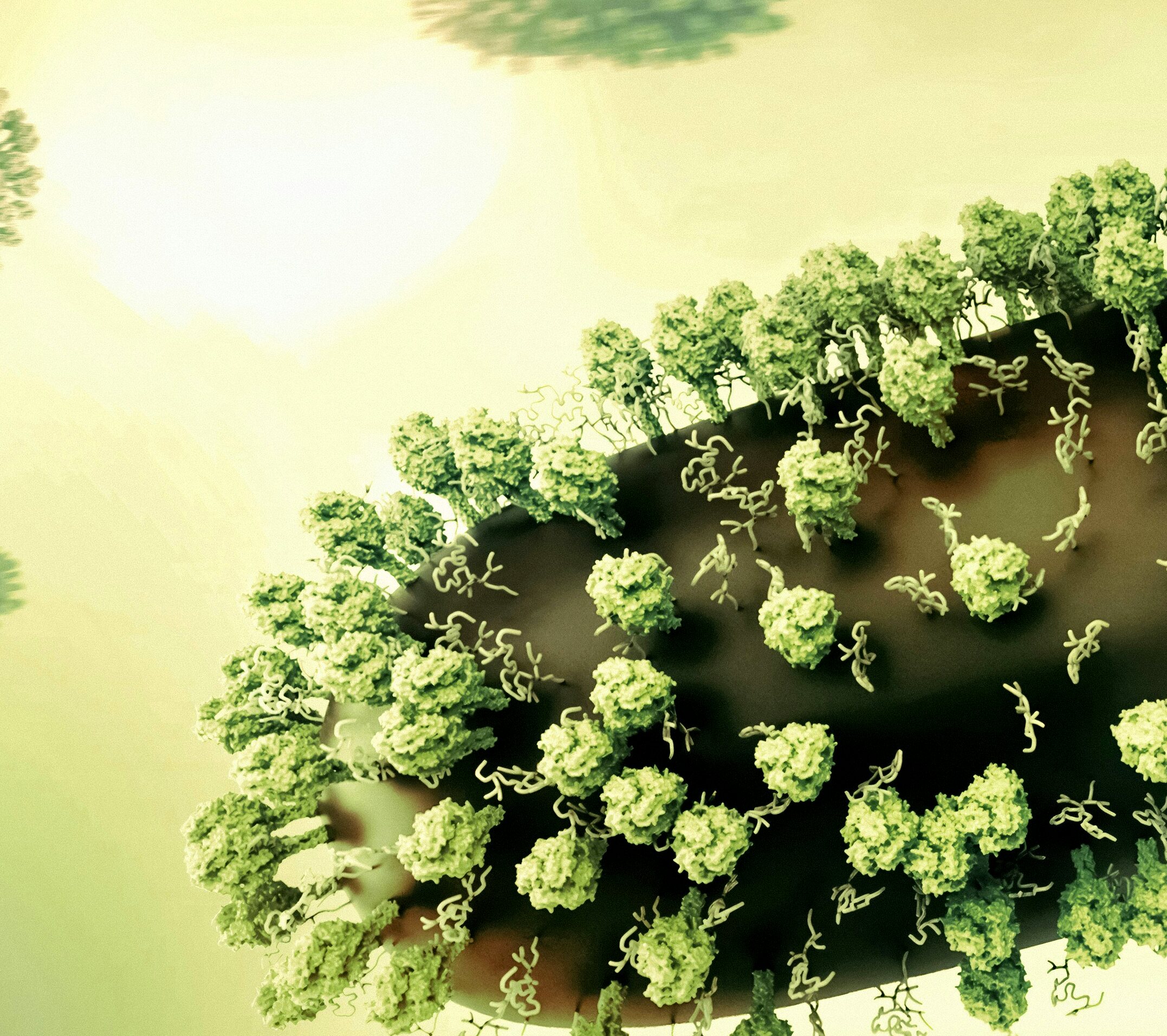
Opiates, a class of drugs including morphine, heroin, and prescription painkillers like oxycodone, have been notorious for their ability to alter brain chemistry, promote addiction, and, according to mounting evidence, contribute to high blood pressure (hypertension) in users. Hypertension, a silent killer responsible for strokes, heart attacks, and chronic kidney disease, affects over 103 million Americans - an alarming statistic that has driven public health experts to reevaluate the impact of substance abuse on this burgeoning problem.
The connection between opiate use and hypertension is multifaceted. Firstly, opiates constrict blood vessels, which can lead to increased resistance and raised systolic blood pressure readings. Secondly, opiate users are more likely to exhibit behaviors such as sedentary lifestyles, poor nutrition, and smoking, all risk factors for developing high blood pressure. Lastly, certain prescription painkillers - like codeine, hydrocodone, and fentanyl - contain high doses of sodium, which can contribute to fluid retention and further raise blood pressure levels.
Navigating the intricate relationship between opiates and hypertension requires a keen understanding of blood pressure measurement techniques and implications. According to the American Heart Association, the appropriate blood pressure cuff size should be 80-100% of the circumference of the upper arm - typically measured midway between the shoulder and the elbow crease. Using a cuff that is too small or too large can yield inaccurate results and misdiagnosis.
For those struggling with opiate addiction who concurrently manage high blood pressure, addressing both issues is paramount for long-term success. The most effective approach combines medication-assisted treatment (MAT), behavioral therapy, and lifestyle modifications like regular exercise, a balanced diet, and stress management techniques. It's important to note that while some MAT medications - like methadone and buprenorphine - can elevate blood pressure in some patients, appropriate monitoring and adjustments by a healthcare professional can help manage any adverse effects.
Another crucial consideration in managing the opiate-hypertension nexus lies in understanding the hypertension epidemiology. Data from the Centers for Disease Control and Prevention (CDC) reveal that non-Hispanic Black adults have significantly higher rates of hypertension compared to their White counterparts - roughly 45% versus 29%. This racial disparity may be partially attributed to social determinants like lack of access to quality healthcare, food deserts, and environmental pollution - all factors that exacerbate health risks for disadvantaged populations.
As researchers continue to unravel the complexities of opiate usage and blood pressure dynamics, it is becoming increasingly clear that addressing this public health crisis will require a comprehensive and multi-faceted approach. By educating individuals about proper blood pressure measurement techniques, targeting resources to affected communities in need, and employing evidence-based treatments for both opiate addiction and hypertension management, we can begin to chip away at this seemingly insurmountable challenge.
In an unexpected twist in the opiate saga, recent studies suggest a potential link between Benadryl (diphenhydramine) and increased blood pressure levels. This antihistamine - often used to treat allergies - can cause drowsiness, dry mouth, and restlessness when taken in excessive quantities or by those with underlying heart conditions. While more research is needed to fully understand this association, it serves as yet another reminder of the intricate dance between substances and cardiovascular health.
In conclusion, the tangled web woven by opiate usage and blood pressure regulation is a testament to the delicate balance required for optimal human function. By raising awareness about these interconnected issues, advocating for equitable resource allocation, and fostering collaboration among healthcare providers, policymakers, and community organizations, we can embark on a collective quest towards a healthier future.